As we march towards an aging society, characterized by a substantial portion of the population surpassing 65 years of age, the landscape of healthcare delivery undergoes a profound transformation. By 2030, projections indicate that 20% of the population will fall into this age bracket,1 ushering in a new era where addressing the unique healthcare needs of older adults becomes paramount.
Central to this shift is the recognition of reduced physical activity among the elderly, making traditional healthcare visits to centralized facilities increasingly challenging. Moreover, with over 90% of older adults expected to grapple with chronic diseases, and 70% experiencing multiple chronic conditions simultaneously,2 the focus shifts from acute treatment towards proactive disease management.2 In this context, ensuring sustainable healthcare costs becomes imperative to provide routine access to diagnostics and therapeutics for aging populations.
In response to these evolving needs, the concept of point-of-care diagnostics emerges as a beacon of hope.3 Rather than requiring older adults to navigate the hurdles of visiting centralized healthcare facilities, point-of-care diagnostics bring the diagnostic lab directly to the patient.4 This paradigm shift not only enhances convenience and accessibility but also facilitates proactive disease management by enabling timely interventions and monitoring.
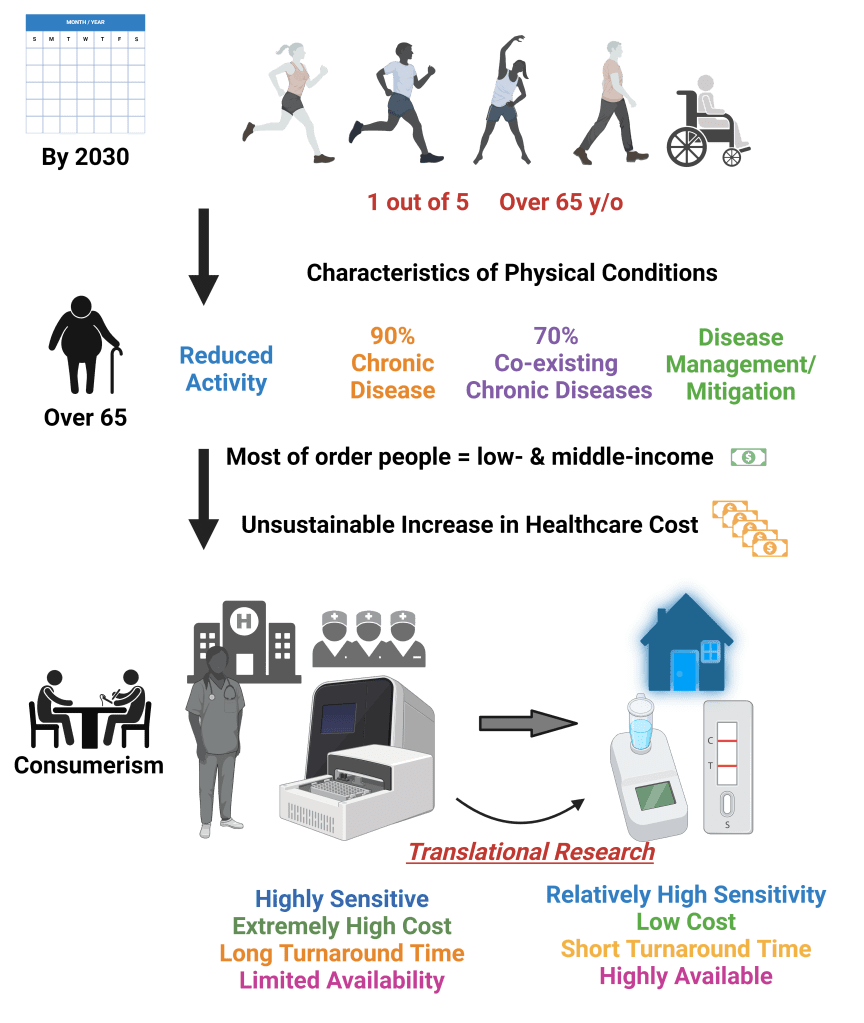
The significance of translational research cannot be overstated in this context. By bridging the gap between sophisticated, lab-based machinery and portable or wearable devices, translational efforts hold the key to unlocking the full potential of point-of-care diagnostics. These portable solutions empower healthcare providers to deliver timely and tailored interventions, empowering older adults to take control of their health and well-being.
Moreover, the advent of point-of-care diagnostics has far-reaching implications beyond the realm of aging populations. From rural communities with limited access to healthcare infrastructure to emergency settings demanding rapid and accurate diagnostics, these portable solutions democratize access to healthcare, ensuring equitable provision of services to all.
In conclusion, as we confront the challenges and opportunities presented by an aging society, the adoption of point-of-care diagnostics emerges as a cornerstone of modern healthcare delivery. By bringing diagnostics directly to the patient and leveraging translational research to drive innovation, we can empower older adults to lead healthier, more independent lives while fostering sustainability in healthcare costs. It’s time to embrace the promise of point-of-care diagnostics and chart a course towards a future where healthcare is truly accessible to all, regardless of age or circumstance.
Reference
- National Council on Aging. Chronic Inequities: Measuring Disease Cost Burden Among Older Adults in the U.S. A Health and Retirement Study Analysis. Page 5, Figure 2. April 2022. Found on the internet at https://ncoa.org/article/the-inequities-in-the-cost-of-chronic-disease-why-it-matters-for-older-adults
- Landers, S. H. (2010). Why health care is going home. New England Journal of Medicine, 363(18), 1690-1691.
- Jani, I. V. (2013). How point-of-care testing could drive innovation in global health. The New England journal of medicine, 368(24), 2319.
- Valera, E., Jankelow, A., Lim, J., Kindratenko, V., Ganguli, A., White, K., … & Bashir, R. (2021). COVID-19 point-of-care diagnostics: present and future. ACS nano, 15(5), 7899-7906.